Glubran 2: AVM
Ezio Lanza MD
We are now going to look at some case reports concerning the use of Glubran®2 in Arteriovenous and Venous Malformation, a wide area that Park and Young, among others, have successfully managed to classify in a chapter of their book “Congenital Vascular Malformations: A Comprehensive Review of Current Management”.
Park, Kwang & Do, Young. (2017). Angiographic Classification: Arteriovenous Malformation and Venous Malformation
The need for a systematic classification arises from the notion that different AVM types behave differently in terms of response, thus attempts have been made to standardize treatment according to AVM type.
CASE 1 – RHINOPHARYNX AVM
24 yo man – 1:4 ratio, 0.2ml boluses
A very young man with a small, oval-shaped malformation of the rhinopharynx located right behind the ethmoid bone, which rendered it inoperable. We saw we could gain direct access through the external carotid artery, performed a selective angiography, and then proceeded to distally place a micro-catheter and injected 0.2 ml of standard glue mixture, thus achieving full exclusion. As these kind of malformations are mostly congenital and do not tend to grow much over time, the successful result was confirmed at 2-years follow up.

CASE 2 – RIGHT THORACIC WALL AVM
28 yo man – multiple treatments
Such a large AVM usually requires multiple treatments: we started with selective catheterization of a malformed vessel arising directly from the right subclavian artery and made multiple attempts at using a high-density glue mixture to embolize different parts of the malformation. In these cases, surgery would be very invasive and the AVM would just grow back, so liquid embolic agents are our only option. The goal is to reduce the symptoms, do as little harm as possible, and go back at a later time when symptoms resurface. In our case, we treated the patient again after one year.
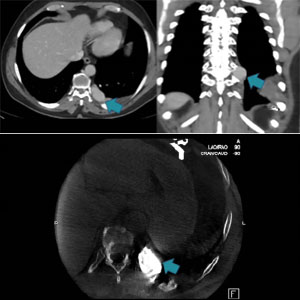
CASE 3 – LEFT THORACIC WALL
60 yo man
This is a very interesting case that goes to show how things do not always go as planned. The patient had a very symptomatic AVM with high-risk bleeding that was also eroding part of the bone cortex. A previous embolization with coils had produced no significant results. We performed an angiography of the left intercostal artery and used selective catheterization to enter the sac, then glued distally, creating a blockage. We kept injecting glue until there was a very low residual flow from the malformation. As shown in the bottom left picture, the result was very satisfactory, however, we later discovered that some glue had migrated to a spinal artery, thus provoking ischemia of the spinal cord. Luckily, using the small bolus technique meant that only a reduced amount of glue had migrated, and the damage was not severe. At follow up, a month ago, the patient exhibited only mild symptoms.
CASE 4 – GLUTEAL AVM
Another large AVM that we treated with coils first, then with glue. Because such cases need to be treated repeatedly, communication with the patient becomes very important: we create a relationship and monitor symptoms regularly so that we decide together with the patient when it is time to intervene again.

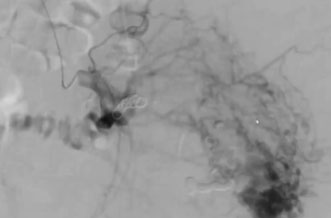
CASE 5 -PELVIC CHO TYPE 2 AVM
54 yo man – Large venous outflow 1:4 Glubran + Amplatzer plug
In this case, we needed to block the outflow from a large venous sac, so we used triple access (one arterial and two venous), placing a 32 mm Amplatzer plug on the large venous outflow of the AVM, This way we could operate with no risk of non-target embolization. We injected small amounts of glue, some of which gathered in high-density concentration just below the plug, which effectively stopped it from migrating into the pulmonary circulation system. This is also called the “Pressure Cooker Technique” , which can be used with liquid embolic agents. As the bottom picture shows, the final result was excellent. severe. At follow up, a month ago, the patient exhibited only mild symptoms.
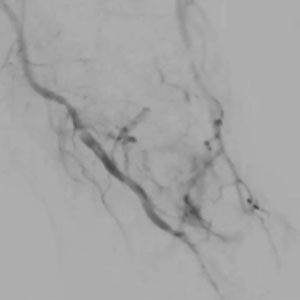
CASE 6 – FOREFOOT AVM
Woman (35) – 0.1 ml Glubran®2 1:3 in the posterior tibial. Manual compression of the digital arteries
This was a wide AVM, similar to a sponge, which we embolized with a very dense mixture through a distally placed catheter while applying manual compression to the digital arteries. As you can see in the picture, digital circulation has been preserved. The result was satisfactory even though we noticed that a small part of the malformation appeared still vascularized. In treating AVMs, in fact, it is important to focus on the symptoms rather than on the image: striving for perfection will likely lead to nontarget embolization and its consequences.

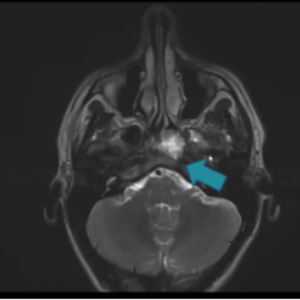
CASE 7 – EMERGENCY EMBOLIZATION LARGE FACIAL AVM BLEEDING
This is a case of large AVM arising from the external carotid artery, which was bleeding into the mouth and therefore required emergency treatment. Nontarget embolization occurred, with some glue migrating to the internal carotid artery and displacing into the brain, provoking stroke-like symptoms. Thanks again to the sandwich technique and the glue having been injected in small boluses, the symptoms disappeared within a week. And at 3-months follow up, the signs of the non-target embolization had disappeared.
For those of you wishing to learn from our mistakes, we have published an open-access full report on this case, under the following title: “Full recovery after non-target cerebral embolization.”
Lanza E, Gennaro N, Poretti D, et al. Full recovery after non-target cerebral embolization of n-butyl-cyanoacrylate occurred during emergency treatment of a facial arteriovenous malformation. CVIR Endovasc. 2019;2(1):20. Published 2019 Jun 29. doi:10.1186/s42155-019-0063-3




